PAD Quick Reference
Use this web-based quick guide to see information about diagnosing and managing PAD at a glance.
Download a print-friendly PDF of this guide.

Background
-
Peripheral Artery Disease (PAD) is atherosclerotic artery disease, most typically in lower extremity
-
PAD Guideline Directed Medical Therapy (GDTM) used only 30-40% due to clinical knowledge gaps
-
There is significant evidence that adherence to 4 recommended therapies reduces risk of adverse cardiovascular (36%) and limb events (44%)3
-
Examples of the 4 GDTMs include: aspirin, statin medications, ACE inhibitors, and smoking cessation
-
-
Only 10% of patients with PAD exhibit classic claudication
-
~50% are asymptomatic
-
~40% have atypical leg symptoms (i.e. knee pain, hip pain, etc)
-
-
African Americans have twice the risk compared with other races
-
High annual mortality of 5-7% in PAD patients without critical limb ischemia
Diagnosis
-
Risk Factors: Age > 65, tobacco use, DM, HTN, hyperlipidemia, AAA, known atherosclerotic disease, and family history of PAD
-
History Clues: Lower extremity pain, more specifically claudication, other non-joint related exertional leg symptoms, impaired walking
-
Claudication = reproducible discomfort (cramping, aching, pain) or fatigue in the muscles of the lower extremity occurring with exertion and relieved within 10 minutes of rest
-
-
Physical Exam: Diminished pulses, vascular bruits, pallor, rubor, non-healing wounds, any evidence of lower extremity gangrene
-
Differential diagnosis may be broad and includes:
-
Venous ulcer, symptomatic Baker’s cyst, local trauma, neuropathy, infection, small artery occlusion (microangiopathy), drug reaction/ toxicity, autoimmune injury, inflammatory disorder, spinal stenosis, nerve root compression, arthritis of hip, ankle or foot, chronic compartment syndrome
-
Testing and Assessment for Intervention
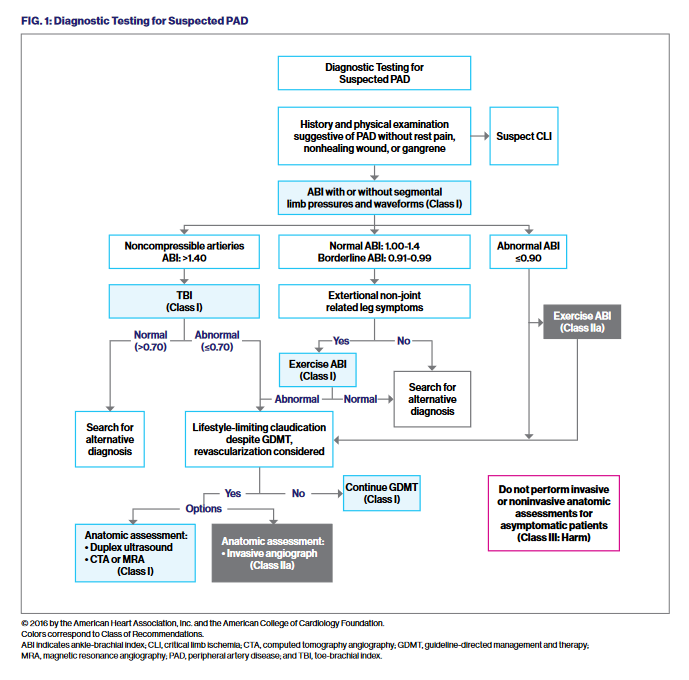
See also figure 1
Diagnosis and Assessment for PAD |
Test to Order |
Indication |
Next Steps Based on Result |
|
Diagnosis |
Ankle Brachial Index (ABI): 1.0-1.39 (normal range) |
If history and/or exam suggestive of PAD
Screening is reasonable if asymptomatic, but PAD risk factors present |
ABI = 1.0-1.39: Look for other causes of symptoms/abnormal exam ABI = 0.91-0.99: Possible PAD. Obtain exercise treadmill ABI or 6 MWT* ABI <0.90: GDMT* if CLI* not present ABI >1.40: Obtain Toe Brachial Index (TBI). TBI <0.70 indicates PAD If CLI suspected and ABI non-compressible, obtain TBI with waveforms or toe perfusion pressure |
|
Anatomical Assessment |
CT Angiogram, or Magnetic Resonance Angiogram |
Indicated if considering revascularization procedure or surgery |
Revascularization should be considered for ALI, CLI, or symptomatic iliac disease, or infrainguinal disease that significantly impairs functional status/QoL* despite GDMT and exercise therapy |
*6 MWT: 6 minute walk test
GDMT: Guideline directed medical therapy
ALI: acute limb ischemia
CLI: Critical leg ischemia
QoL: Quality of Life
Click on the image below to open in a new tab.
Management/Treatment Specifics
Goals
- Eliminate/reduce claudication to improve mobility, functional status, and health-related QoL
- Reduce risk of fatal ischemic cardiovascular events and limb loss
PAD Management Checklist for Front Line Providers
Management |
Intervention |
Frequency/Dosing |
Considerations |
|
Prior to any vascular intervention |
Asymptomatic PAD (ABI < 0.9): |
ASA 81 mg daily or Plavix 75 mg daily |
|
|
Symptomatic PAD: |
ASA 81 mg |
ASA and Rivaroxaban may improve CV outcomes, with modestly If there is an increased risk of bleeding, ASA or Clopidogrel can be Dual antiplatelet therapy (DAPT) generally not recommended for |
|
|
Post-vascular intervention |
ASA + Rivaroxaban |
ASA 81 mg daily plus |
ASA and Rivaroxaban may reduce risk of adverse CV and limb If risk of bleeding is increased, DAPT with ASA and Clopidogrel may |
|
Cilostazol |
Reduces claudication, increases walking |
100 mg BID |
Side effects: Headache, palpitations, and diarrhea Contraindicated in presence of Heart Failure and/or EF <40% |
|
Hypertension management |
Target blood pressure: <130/<80 |
Monthly until controlled, then every 3-6 months |
No preferred agent in absence of other disorders (DM, CKD, CHF) Beta-blockers not associated with worsening claudication First line is often ACE inhibitors |
|
Diabetes management |
HbA1c <7% (unless risk > benefit) |
Controlled: q 6 months Poorly controlled: q 3 months |
Intensify medications to optimize control Biannual foot exam with monofilament test |
|
Lipid management |
LDL target <70 mg/dl |
Ongoing treatment |
Moderate or high intensity statin therapy, indicated for all PAD Ezetimibe ($) may be added to achieve LDL goal PCSK-9 inhibitors ($$$) may reduce CV and adverse limb events |
|
Tobacco screening and cessation |
Screen all patients annually with regular follow up to ensure cessation Refer to smoking cessation program Medication options include buproprion, varenicline, or nicotine replacement |
Active smokers: address every visit |
Provide a medication prescription even if patient not ready to fill, so Detailed discussion on “what will happen to your health and limbs if |
|
Exercise program |
Supervised or home-based |
3-5 sessions per week |
Home Based Exercise performed 3-5x/week, beginning possibly Increasing walking per session by 5 min per week, until patient Treadmill-based exercise therapy program for patients with PAD: |
|
Revascularization |
Claudication severity, presence of iliac disease, and QoL drives revascularization decision <10-15% progress to CLI over 5 years Note: 0.15 increase in ABI is considered significant post-procedure |
Performed in conjunction with GDMT and exercise therapy |
Iliac disease: Generally treated with revascularization Below Iliac disease: Generally, GDMT + Exercise Therapy are initial When CLI present, endovascular and/or surgical procedures used Surgical patency rates higher than endovascular procedures, but Post-procedure follow-up with periodic ABI measurements and, in |
NOAC: Novel Oral Anticoagulant, CLI: Critical leg ischemia, QoL: Quality of Life, GDTM: Guideline Directed Medical Therapy
When to Refer to a Vascular Specialist
-
Debilitating claudication
-
Lifestyle limiting activity
-
Diabetes and foot wound
-
Non-healing foot wounds
-
Known PAD and foot wound
Additional Management Considerations
Supervised/Home Exercise Program
-
Effectively reduce claudication and atypical symptoms, improve both functioning and QoL, alone or in conjunction with revascularization
-
Other exercise strategies include upper-body ergometry and cycling for patients with leg amputations
Foot Care for Patients with Diabetes
-
Biannual foot exams including pulses/perfusion, use 10 g monofilament and either temp, pinprick, vibration, or ankle reflexes to detect neuropathy
-
Refer patients with PAD to podiatrist
-
If foot ulcer present, refer to vascular specialist
Minimizing Risk of Tissue Loss
-
Prevention: patient education regarding healthy foot behaviors (e.g., daily feet inspection; foot care and hygiene, including safe toenail cutting strategies; avoidance of barefoot walking, proper shoes)
-
Prompt diagnosis and treatment of infections and other foot disorders
-
Suspect if patient has local pain, tenderness; inflamatory reaction around wound, pretibial edema; discharge or odor, or signs of a systemic inflammatory response
-
Treatment of deep soft-tissue infections typically requires prompt surgical drainage; vascular imaging and timely revascularization
-
-
Goal: complete wound healing
Acute Limb Ischemia is a medical emergency typically requiring prompt anticoagulation, emergency consultation with vascular specialist, and thrombolysis or thrombectomy for viable limbs.
PAD: Clinical Integrated Care Considerations and Information
Refer to Vascular Medicine/Cardiology
-
Assistance in managing coexisting PAD risk factors, such as HTN, lipid disorders
-
Pre-operative assessment of high risk patients
-
Confirm diagnosis of PAD when symptoms atypical and/or normal/borderline noninvasive tests
-
Phone number: 212-241-9454 to request appointment with Dr. Olin at The Lauder Family Cardiovascular Ambulatory Center
Refer to Surgery (i.e. Vascular Specialist)
-
Determine the most appropriate diagnostic testing and arrangement
-
Revascularization in patients with refractory symptoms despite GDMT
-
Manage acute and critical limb ischemia
-
Treatment of non-healing skin and soft tissue infections and non-healing wounds
- Diagnostic Testing Available by Location
-
All Locations: ABI Testing, Exercise ABI, Toe Brachial Index (with waveforms), Toe Perfusion Pressure
-
Mount Sinai West and Mount Sinai Downtown Only: Transcutaneous 02 pressure
-
Hospital |
Location of Vascular Surgery/Outpatient Wound Care |
Vascular Surgery Phone Numbers |
|
The Mount Sinai Hospital |
17 East 102nd Street, 4th Floor, New York, NY 10029 1190 Fifth Avenue, 1st Floor, GP-1 Center, New York, NY 10029 |
212-659-8554 212-241-5315 |
|
Mount Sinai Morningside |
440 West 114th Street, Ambulatory Care Center, New York NY 10025 CVI 2nd Floor Suite 220 OR ACC 1-1st Floor |
212-523-3360 |
|
Mount Sinai West |
425 West 59th Street, 7th Floor, New York, NY 10019 |
212-523-4797 |
|
Mount Sinai Queens |
Mount Sinai Queens Pavilion 25-20 30th Avenue, 5th Floor, Astoria, NY 11102 |
718-808-7777 |
|
Mount Sinai Downtown |
10 Union Square East, 2nd Floor, Suite 2N, New York NY 10003 |
212-844-5559 |
|
Mount Sinai Brooklyn |
MS Outpatient Vascular Office 3131 Kings Hwy, Room LL07 |
718-677-0109 |
|
Mount Sinai South Nassau |
1420 Broadway, 2nd Floor, Hewlett, NY 11557 |
516-374-8682 Wound Care: 516-764-4325 |
** Wound Care is offered at all locations, except MS-South Nassau sees patients at their Wound Care Center
Refer to Interventional Radiology
-
Diagnostic angiography and therapeutic catheter-based interventions in symptomatic PAD
Hospital |
Location |
Phone Numbers |
|
Mount Sinai West |
1000 Tenth Avenue, 2nd Floor, New York NY 10019 |
212-241-4046 (Press 1) |
|
Mount Sinai East |
5 East 98th Street, 12th Floor, New York, NY 10029 |
212-241-4046 (Press 1) |
|
Mount Sinai Queens |
25-20 30th Avenue, 5th Floor, Astoria, NY 11102 |
347-408-8234 |
See website for other locations.
Exercise Program
Supervised Office-Based
-
Offered by Cardiac Rehabilitation @ Mount Sinai Hospital Phone: 212-427-1540
-
Physical Therapy @ Mount Sinai Downtown Union Square, use Epic "PT" referral or Phone: 212-844-8750
Home-Based Exercise
-
Mount Sinai Hospital, Mount Sinai Morningside, Mount Sinai West, and Mount Sinai South Nassau Vascular Surgery locations above provide self-guided handouts
Behavioral Health
-
The prevalence of depression or depressive symptoms in PAD patients is 11-48%, with high rates in female patients, African Americans, and those with advanced disease
-
Annual screening with PHQ2/9 is recommended, with treatment by PCP or behavioral health provider
Care Management Referral
-
Patients who would benefit from nursing education: medication education, diabetic foot care, disease management, or self-management
-
Indicated for patients needing care coordination, history of treatment non-adherence, complex psychosocial needs, and/or avoidable Emergency Room or Inpatient admissions
-
Use “MSHP Care Management” Referral in Epic, email mshpcmreferral@mountsinai.org or phone: 212-241-7228
Home Health Care Referral
-
Home-based care may be arranged using "Consult to Visiting Nurse Services" order in Epic for the following, but are not limited to:
-
Home-based wound care
-
Home-based visiting physical therapist
-
Home-based nursing education and visits
-
References
1. Gerhard-Hermann MD et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease.
J Am Coll Cardiology 2017:69:1465-1508
2. Cambia U. et al, Peripheral Arterial Disease: Past Present and Future. Am J Med 2019;132:1133-41
3. Armstrong E et al. J Am Heart Assoc 2014;3:e000697.
4. Eikelboom JW et al. N Engl J Med. 2017 Oct 5;377(14):1319-1330,
5. Anand SS et al. Lancet. 2018 Jan 20;391(10117):219-229.
6. Bonaca MP et al. N Engl J Med. 2020;382:1994-2004
7. Mount Sinai Health System Experts: Dr. Jeffrey Olin, Dr. Peter Faries, Dr. Soma Brahmanandam
Next Steps
Explore Team-Based Care services available to you and your practice as a member of MSHP's Clinically Integrated Network.
Need a consult? Connect with our experts