Measurement
Home blood pressure monitoring is important to identify “white coat hypertension” and "masked hypertension" (normal reading in office but elevated reading at home).
How to take an accurate blood pressure reading:
- Sit in quiet room at a comfortable temperature
- No smoking, coffee, or exercise for 30 minutes prior
- Empty bladder
- Relax for 3-5 minutes
- Back supported and feet flat on the floor
- Arm bare and resting, mid-arm at the heart level
- Cuff selected to fit arm size (small, usual, large)
- Use a validated electronic upper-arm cuff or manual auscultatory
- Take 3 measurements at 1 minute intervals
- No talking during and between measurements
- Use the average of the last 2 measurements
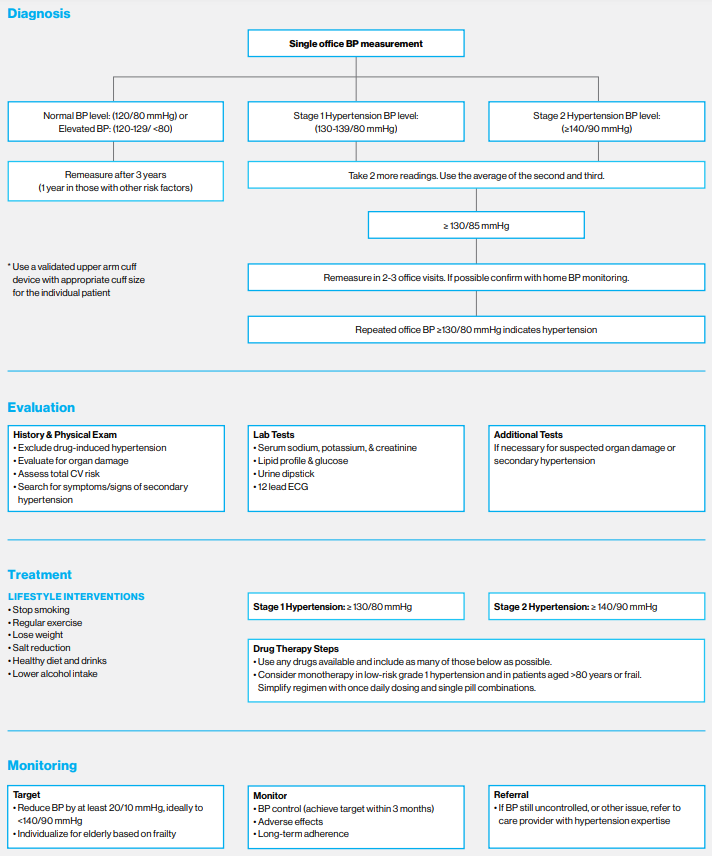
Diagnosis
Diagnose hypertension when either of the following criteria are met:
- Office BP of at least 140/90 over 2-3 visits at 1-4 week intervals*
- Single office visit BP of at least 180/110
*Confirm with out-of-office measurements
Hypertension Categories
| Office measurement | Home measurement | ||
|---|---|---|---|
| SBP | DBP | ||
| Normal BP | <120 | <80 | <120/80 |
| Elevated BP | 120-129 | 80-89 | ≥120-129 and/or <80 |
| Stage 1 hypertension | 130-139 | 80-89 | ≥130-139 and/or ≥80-80 |
| Stage 2 hypertension | ≥140 | ≥90 | ≥135 and/or ≥85 |
Note: Home BP of 135/85 is equivalent to office BP of 140/90
Initial Evaluation
- Confirm diagnosis with out-of-office measurements
- Laboratory testing should include basic metabolic panel, lipids, U/A, and EKG, with additional testing, as warranted, to detect/confirm hypertension-mediated organ damage (i.e. retinal imaging)
- Consider evaluation for secondary causes (primary aldosteronism, renovascular, drugs/meds, sleep apnea, CKD, and others), if indicated
- Calculate 10-yr risk of a first ASCVD event
-
Note: CKD patients are high-risk patients
-
- Assess other relevant comorbid conditions and complications of HTN
Pharmacology
Management includes lifestyle modification promoting a healthy diet, limited alcohol and caffeine consumption, weight reduction, tobacco cessation, regular exercise, stress management, and avoiding medications/drugs that increase blood pressure.
Patients with BP between 130-139/80-89 and 10-year ASCVD risk <10% can be managed with non-pharmacologic therapy, while those with risk >10% should also receive medication. A BP decrease of 20/10 mmHg is associated with a 50% decrease in cardiovascular risk.
Medication Initiation Threshold
| Blood Pressure | Risk profiles & comorbid disorders |
|---|---|
| ≥ 140/90 | Any ASCVD |
| ≥ 130/80 | ACSVD risk ≥10% Known CAD, prior stroke or TIA HFpEF HFrEF and achieved maximally tolerated doses of GDMT Diabetes mellitus Chronic kidney disease Chronic obstructive pulmonary disease |
- Single-pill combinations should be used as the first line of pharmacological treatment whenever available as they are associated with better adherence and persistence than multi-pill regimens
- Use once-daily regimens providing 24-hour blood pressure control, whenever possible
- Screen for and address behavioral health disorders and social determinants of health
- Both office-based and home blood pressure measurements are useful to guide treatment
- Evaluate/promote medication adherence at each visit, prior to escalation of treatment
- Prescribe 90-day fills if appropriate
- Both video and telephone-only visits can be effective for hypertension management
- Have patients secure readings leading up to appointment
- Providers should appropriately document in EMR (may be utilized for quality measurement)
Remember that the MSHP Pharmacy Team is available to assist with chronic disease management
Resistant Hypertension
Resistant hypertension is defined as persistent, appropriately measured, BP ≥140/90 mmHg in a patient treated with 3 or more antihypertensive medications, including a diuretic, on optimal (or maximally tolerated) doses OR controlled BP on 4 agents.
Treatment
- Optimize lifestyle modification and medication adherence
- Reassess possible secondary causes of hypertension
- If GFR <30 or volume overloaded, use a loop diuretic
- Add a low dose of spironolactone if K <4.5 mmol/L and GFR >45 ml/min
- If contraindicated/not tolerated, use eplerenone or potassium-sparing diuretic (assess renin/aldo level)
- Other additional treatments include doxazosin, clonidine, hydralazine, beta-blockers, or other available antihypertensive class not already in use
- Giving one antihypertensive medication in the evening may address end-of-dose effect
When to Refer
Consider referring the patient to specialty care in the below cases.
Nephrology
- Resistant hypertension
- To clarify the cause and treatment of co-morbid CKD and management of related complications
Endocrinology
- Evaluation and treatment of endocrine causes of secondary hypertension
- Treatment of other poorly controlled endocrine disorders that impact HTN care (DM, hyper/hypothyroidism, hypogonadism)
Cardiology
- For treatment of concomitant cardiac disease (CAD, HF, Afib)
- Assessment/treatment of renovascular hypertension
Team-Based Care
Leverage the support of additional care team members to effective manage patients with chronic conditions. Available services include:
- Clinical pharmacists
- Certified Diabetes Educators (CDE/Wellness Coaches)
- Care management
- Behavioral health
Remote Patient Monitoring
Mount Sinai Health Partners Condition Management Program is available live at over 30+ primary care and specialty practices across the system for patients with uncontrolled hypertension, depending on patient insurance. Patients receive Bluetooth-connected blood pressure cuffs and are managed by a team of clinical pharmacists and dietitians in collaboration with referring physicians.
Refer patients using the “Referral to Condition Management Department” order in Epic.
Cost Sharing for Services
- Traditional Medicare: 80/20 coinsurance split
- Medicare + Secondary: 20% coinsurance is typically offset by secondary
- Healthfirst Medicaid and UMR are covered
Next Steps
- Review the MSHS Ambulatory Care Pathway for Hypertension for more in-depth guidance on evidence-based best practices
- Print and share resources with your patients to empower them to meet their care goals
- Check out Hypertension Condition Management Tips for quick takeaways to keep you up-to-date on management guidelines