Mount Sinai Heart Failure Ambulatory Care Pathway
The Mount Sinai Ambulatory Care Pathway for Heart Failure provides in-depth, evidence-based guidance for primary care physicians and the collaborative team managing heart failure outpatients. Included are best practices and practical tips for clinicians, and while the focus is on HFrEF, there are also callouts for HFpEF and RHF throughout. Guidance for telemedicine is also given. A number of helpful charts and diagrams are included, as well as visit templates for both initial and subsequent follow-up visits.
Click on the links below to jump to a section, or scroll through the document. You can also download a print-friendly PDF here.
Contents
Medications
Guidelines for Initial Medication Selection
Starting and Target Dosage Chart
HFrEF Medication Notes
HFpEF Medication Considerations
RHF Medication Considerations
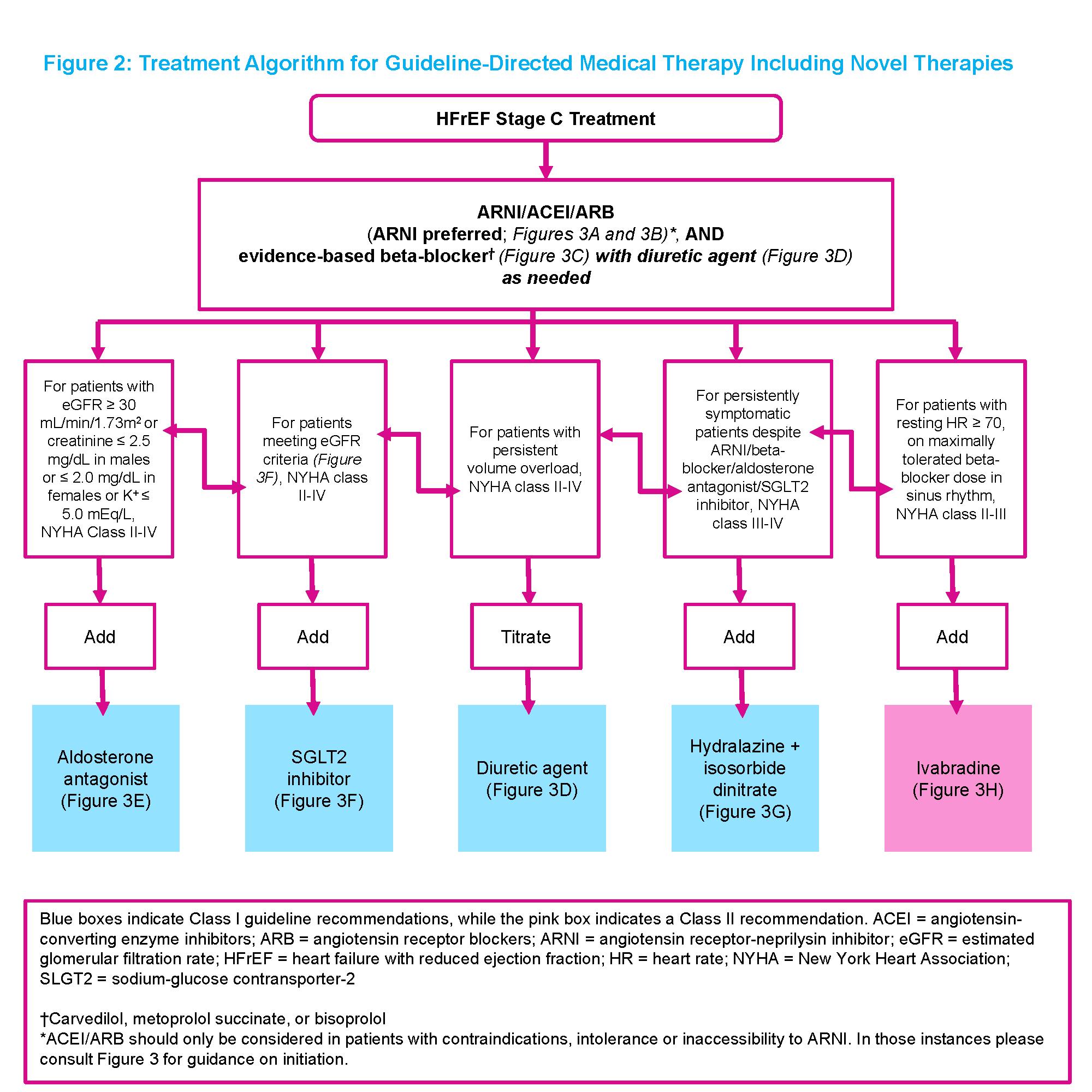
Treatment Algorithm for GDMT
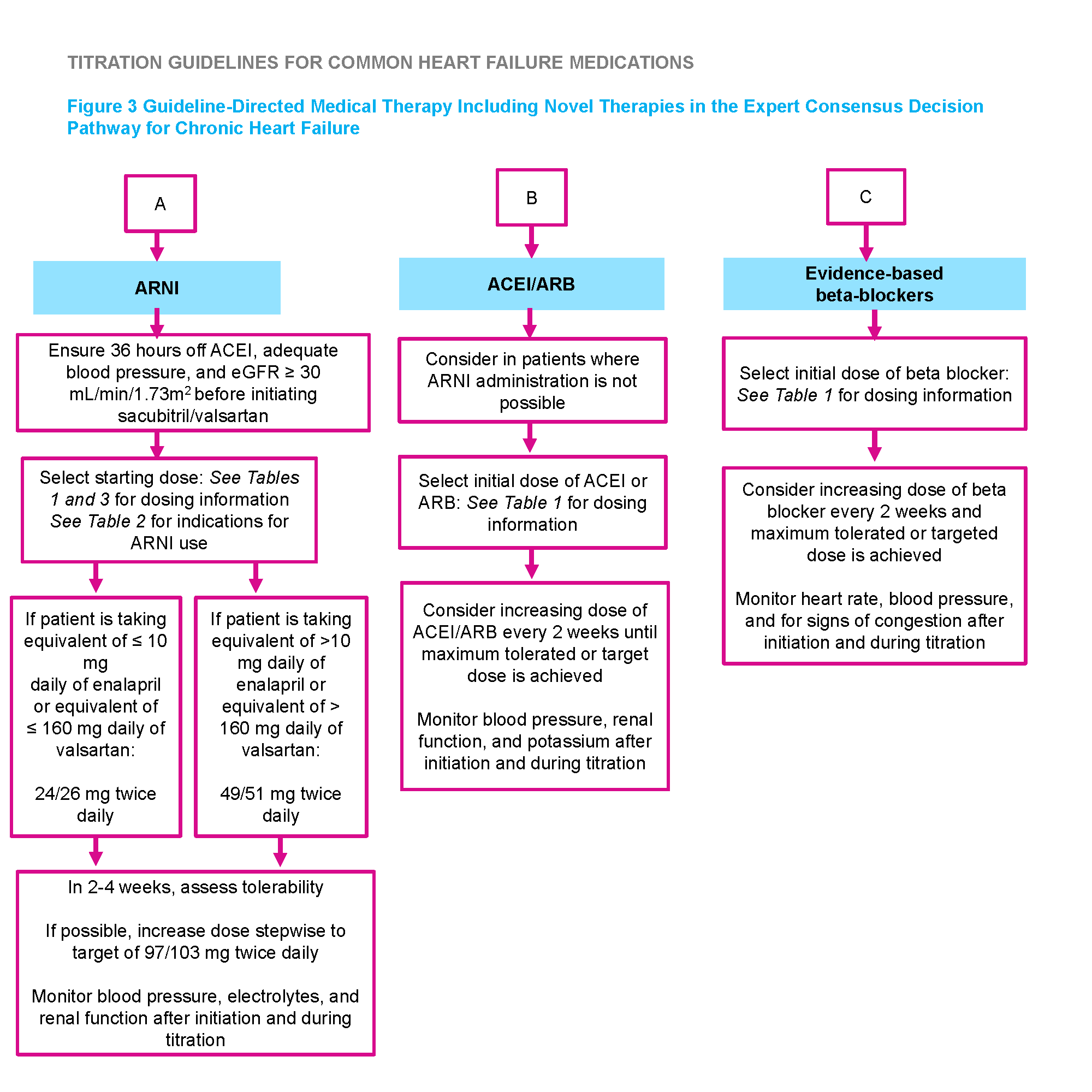
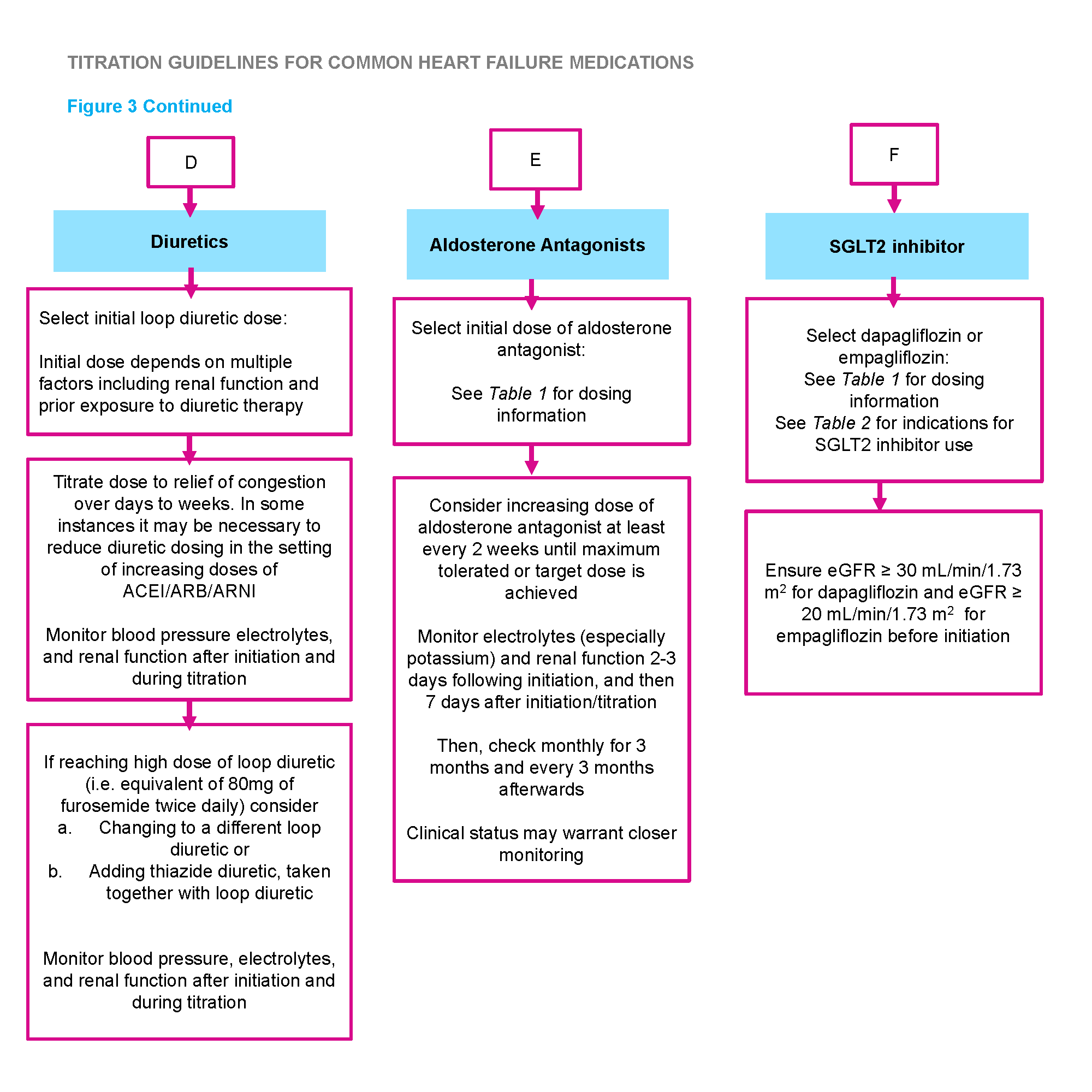
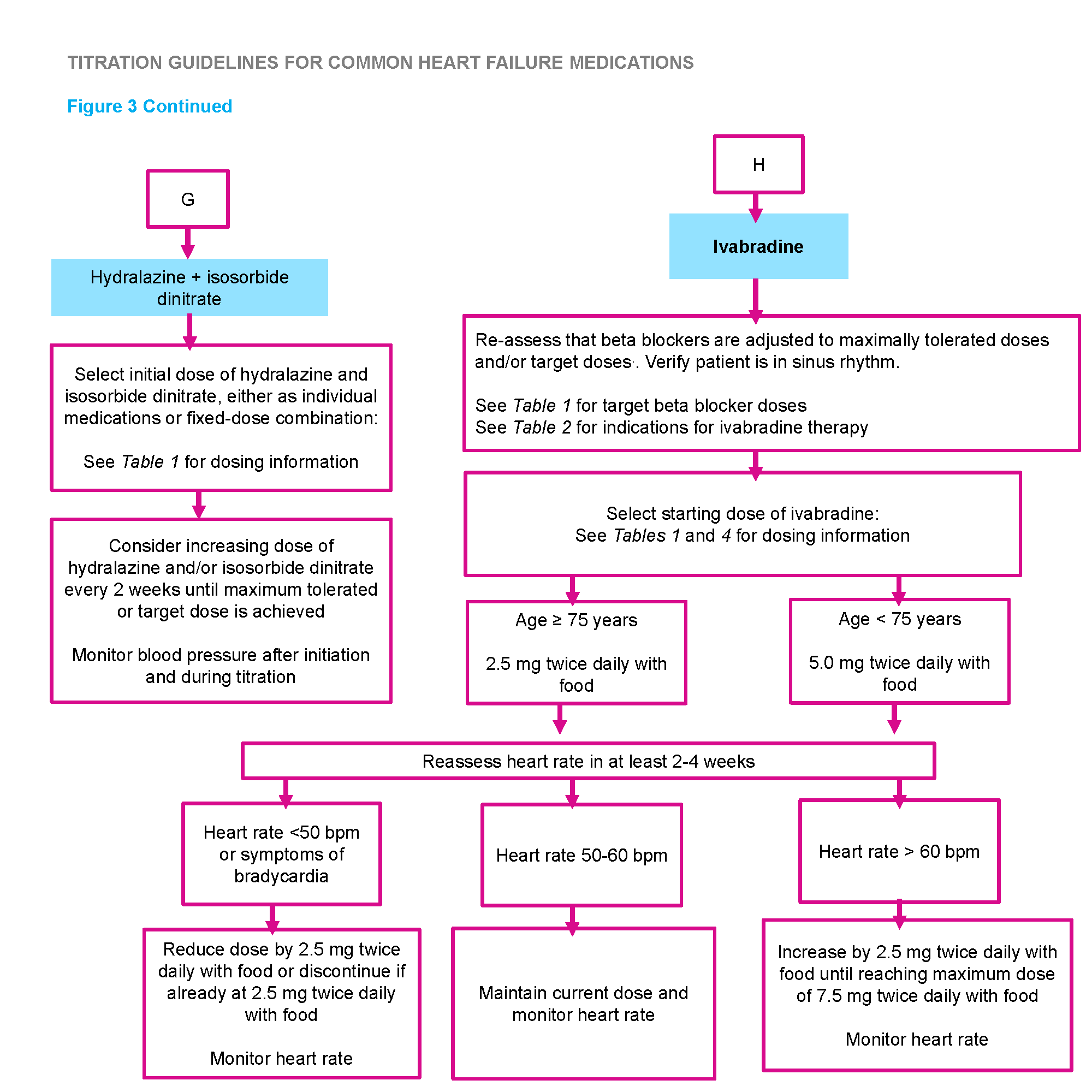
Titration Guidelines
Indications for ARNI and Ivabradine Use
Contraindications and Cautions for Ivabradine
Recommended Starting Dose of Sacubitril/Valsartan
Contraindications and Cautions for Sacubitril/Valsartan
Recommended Indications/Contraindications for Vasodilators
Recommended Indications/Contraindications for Cardiac Glycoside
New Therapies for HFrEF: SGLT-2i
Effect of SGLT-2i on Select CV Outcomes in Placebo Controlled Trials
When to Consider and How to Prescribe
Contraindications and Cautions for Dapagliflozin
HFpEF Considerations
Vaccinations for Heart Failure Patients
Testing & Referral
Use of BNP in Heart Failure
HFpEF BNP Consideration
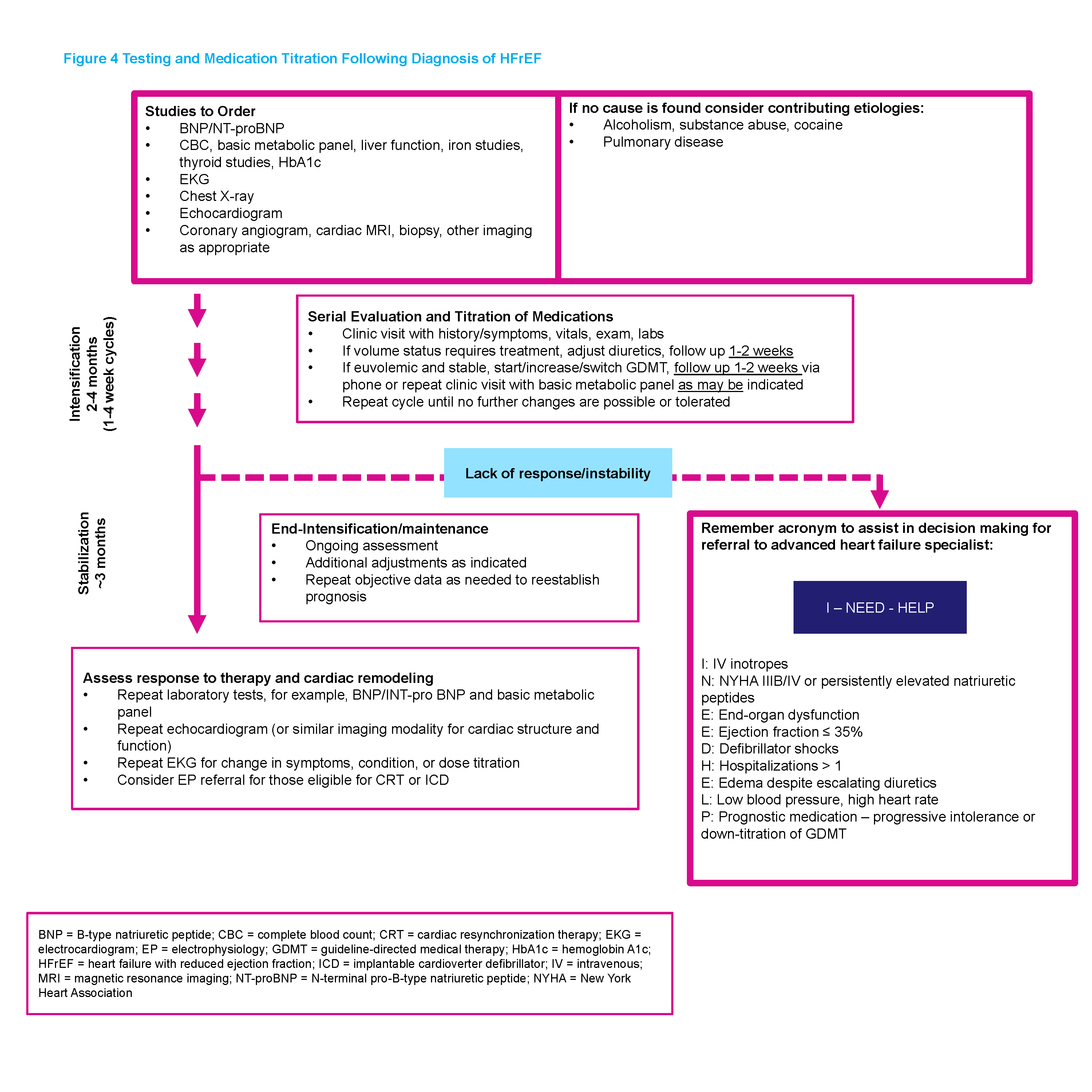
Testing and Medication Following Diagnosis
HFpEF Evaluation and Testing Considerations
RHF Evaluation and Testing Considerations
When to Refer to a Specialist
When to Refer to Device Therapy
When to Refer to Cardiac Rehab
Mount Sinai Heart's Cardiac Rehabilitation Program
Mount Sinai South Nassau's Cardiac Rehabilitation Program
Common Comorbidities and Outcomes on Heart Failure
HFpEF Consideration
Remote Patient Monitoring
Connected Hearts Program
CardioMEMS
Team-Based Care
Pharmacy
Home Health
Care Coordination in Heart Failure at MSHS
Behavioral Health
Certified Diabetes Educators (i.e. Wellness Coaches)
Community Paramedicine
Palliative Care
Rapid Follow Up Clinics
MSHS Heart Failure Rapid Follow Up Clinics Referral Contacts
ReDS Vests
Background
Contents Prevention, Diagnosis, Classification, & Staging of Heart Failure »
- 3 types of heart failure: Heart Failure with Reduced Ejection Fraction (HFrEF), Heart Failure with Preserved Ejection Fraction (HFpEF), and Right Sided Heart Failure (RHF)
- Effective management involves comprehensive, multidisciplinary care
- While this pathway’s major focus is on HFrEF, the content outlines, in appropriate sections, unique considerations for HFpEF and RHF
- Hypertension control, dietary compliance, reduced salt intake apply to all types of heart failure
- The optimal care of patients with HFrEF involves a commitment to guideline directed medical therapy (GDMT) and a multidisciplinary care team
- Primary care has a vital role in providing holistic, person-centered care from first symptoms to end of life
- This document is intended to provide guidance to support primary care providers and the collaborative team on heart failure diagnosis and management
Prevention, Diagnosis, Categorization, and Staging of Heart Failure
« Background Contents Medications »
Prevention
To prevent the initial development of heart failure[1]:
- Effectively manage contributing comorbidities such as diabetes and hypertension
- Regular physical activity (exercising at least 5 d/wk)
- Maintaining a healthy body weight
- Not smoking
- Eating fruits and vegetables (4 servings/day) and moderate alcohol intake (1 drink/day)
Diagnosis
Initial evaluation of patients with symptoms or signs suggestive of HF includes clinical assessment (history and physical exam), electrocardiogram, echocardiogram, blood tests, and chest radiograph.
Early measurement of brain natriuretic peptide (BNP) or N-terminal proBNP levels is suggested in patients with suspected HF in whom the diagnosis is uncertain. BNP levels > 400 ng/L imply a cardiac cause with a sensitivity of 95-97% and a negative predictive value of 90-97%. While BNP levels < 100 ng/L imply a pulmonary cause, BNP levels 100-400 BNP are neither sensitive nor specific for excluding or confirming HF[2,3].
Categorization of Heart Failure 4,5
Heart Failure with Reduced Ejection Fraction (HFrEF)
EF less than or equal to 40%. Mortality benefit proven with Carvedilol, long acting metoprolol (succinate), and bisoprolol, ACE inhibitors/ARBs or Spironolactone
Heart Failure with Preserved Ejection Fraction (HFpEF)
A clinical syndrome in which patients have symptoms and signs of HF, a normal or near normal left ventricular ejection fraction (LVEF at least 50 percent), and evidence of cardiac dysfunction as a cause of symptoms (eg, abnormal left ventricular filling and elevated filling pressures).
- Approximately 50% of patients with heart failure have an EF> 50%, a proportion that is increasing over time. Dominant form of heart failure in the elderly.
- No therapies with proven mortality benefit, unlike HFrEF.
Right Sided Heart Failure (RHF)
RHF is a clinical syndrome in which symptoms and signs are caused by dysfunction of the right heart structures (predominantly the right ventricle [RV], but also the tricuspid valve apparatus and right atrium) or impaired vena cava flow, resulting in impaired ability of the right heart to perfuse the lungs at normal central venous pressures.
- Commonly seen with HFrEF (48%) and HFpEF (20-40%) and, when present, independently associated with increased morbidity and mortality, thus important to ensure actively managed in conjunction with treatment of left heart failure
- Cardiac MRI more accurate than echocardiogram in assessing RV structure and function
- Cardiac catheterization is definitive test, if non-invasive testing inconclusive
Common Classifications of Heart Failure
New York Heart Association (NYHA) Functional Classification
Class |
Functional Capacity: Heart Failure-Related Symptoms According to Activity Level |
Associated HF Severity |
|
Class I |
Patients with cardiac disease (low EF, prior history of systolic or diastolic HF symptoms) but no limitation of ordinary physical activity. Ordinary physical activity does not cause symptoms (undue fatigue, SOB, palpitations). Note: Patient may have mild symptoms on greater-than-ordinary activity, e.g. walking up 4 flights of stairs, carrying heavy objects. |
Very mild or no impairment |
|
Class II |
Patients with cardiac diseases causing slight limitation of physical activity. Ordinary physical activity causes symptoms. Note: “Ordinary” activity generally means: walking (not running) up 1-2 flights, walking a few blocks on flat ground, carrying lightweight objects. |
Mild |
|
Class III |
Patients with cardiac disease causing marked limitation of physical activity. Comfortable at rest. Less-than-ordinary activity causes symptoms. |
Moderate to severe |
|
Class IV |
ANY amount of physical activity causes symptoms. Symptoms may be present at rest. |
Severe |
ACC/AHA Stages of Heart Failure
Stage |
Description |
|
Stage A |
At high risk for HF but without structural heart disease or symptoms of HF |
|
Stage B |
Structural heart disease but without signs or symptoms of HF |
|
Stage C |
Structural heart disease with prior or current symptoms of HF |
|
Stage D |
Refractory HF requiring specialized interventions |
Medications
« Prevention, Diagnosis, Categorization, and Staging of Heart Failure Contents Care Delivery »
Guidelines for Initial Medication Selection in Heart Failure with Reduced Ejection Fraction (HFrEF) Based Primarily on Clinical Findings [4,6,7]
| Starting Dose | Target Dose | |
|---|---|---|
ARNI |
||
| Sacubitril/valsartan | 24/26 mg - 49/51 mg 2x daily | 97/103 mg 2x daily |
ACEI |
||
| Captopril | 6.25 mg 3x daily | 50 mg 3x daily |
| Enalapril | 2.5 mg 2x daily | 10-20 mg 2x daily |
| Lisinopril | 2.5-5 mg daily | 20-40 mg daily |
| Ramipril | 1.25 mg daily | 10 mg daily |
ARB |
||
| Candesartan | 4-8mg daily | 32mg daily |
| Losartan | 25-50 mg daily | 150 mg daily |
| Valsartan | 40 mg 2x daily | 160mg 2x daily |
Beta Blockers |
||
| Bisoprolol | 1.25 mg daily | 10 mg daily |
| Carvedilol | 3.125 mg 2x daily | 25 mg 2x daily for weight <85kg; 50 mg daily for weight =85 kg |
| Metoprolol succinate* | 12.5 - 25 mg daily | 200 mg daily |
Aldosterone Antagonists |
||
| Eplerenone | 25 mg daily | 50 mg daily |
| Spironolactone | 12.5 - 25 mg daily | 25-50 mg daily |
SGLT2 Inhibitors |
||
| Dapagliflozin | 10 mg daily | 10 mg daily |
| Empagliflozin | 10 mg daily | 10 mg daily |
Vasodilators |
||
| Hydralazine | 25 mg 3x daily | 75 mg 3x daily |
| Isosorbide dinitrate | 20 mg 3x daily | 40 mg 3x daily |
| Fixed-dose combination isosorbide dinitrate/hydralazine | 20 mg/37.5 mg (one tab) 3x daily | 2 tabs 3x daily |
Ivabradine |
||
| Ivabradine | 2.5-5 mg 2x daily | 10 mg daily |
Diuretics — Loop |
||
| Bumetanide | 0.5 - 1 mg 1x or 2x daily | 10 mg daily |
| Furosemide | 20-40 mg 1x or 2x daily | 400 mg daily |
| Torsemide | 10-20 mg daily | 200 mg daily |
Digoxin |
||
| Digoxin | 0.125 mg daily | 0.25 mg daily |
| *Unlike immediate-releases metoprolol, metoprolol ER is proven to improve symptoms of heart failure, lower the risk of death from heart failure, and lower the risk of hospitalization due to heart problems. While atenolol is technically another hypertension drug, it doesn't have these additional benefits. | ||
Other HFrEF Medication Notes[4]
- It is recommended that only one of the neurohormonal antagonist (Beta-blocker, ACE, ARB, ARNI, Aldosterone antagonist) be increased at each visit. If the patient is hemodynamically stable, it is generally acceptable to double the dose of these agents when escalating the dose.
- In general, calcium channel blockers should be avoided in HFrEF. However, third generation calcium channel blockers such as amlodipine may be used for blood pressure control in HFrEF. Other calcium channel blockers such as verapamil, diltiazem, and nifedipine should be avoided in patients with HFrEF due to their negative ionotropic effects and studies indicating worse outcomes.
- Anticoagulation indicated if atrial fibrillation present. Choice of agent should be individualized. Routine anticoagulation for heart failure without atrial fibrillation is not indicated.
- If possible, avoid non-steroidal anti-inflammatory drugs (NSAIDs) in HFrEF, because they can cause sodium retention and vasoconstriction and can reduce the effectiveness and increase the toxicity of ACE inhibitors and diuretics.
HFpEF Medication Considerations
- Routine use of nitrates associated with adverse outcomes and should be avoided in HFpEF[3]
- Mineralocorticoid receptor antagonists may be useful adjunctive therapy
RHF Medication Considerations[5]
- Judicious use of diuretics as RHF patients are volume sensitive
Guideline-Recommended Indications for ARNI and Ivabradine Use
Indications for Use of ARNI |
Indications for Use of Ivabradine |
Indications for Use of SGLT2 Inhibitor |
|
HRrEF (EF less than or equal to 40%) NYHA Class II-IV HF Administered in conjunction with a background of GDMT for HF in place of an ACEI or ARB |
HRrEF (EF less than or equal to 35%) NYHA Class II or III HF On maxmimum tolerated doses of beta blocker Sinus rhythm with a resting heart rate of at least 70 bpm |
HFrEF (EF less than or equal to 40%) with or without diabetes NYHA Class II - IV HF Administered in conjunction with a background of GDMT for HF |
Contraindications and Cautions for Ivabradine
Contraindications |
Cautions |
|
HF with preserved ejection fraction (HFpEF) Presence of angina with normal EF Hypersensitivity Severe hepatic impairment (Child-Pugh C) Acute decompensated HF Blood pressure <90/50 mm Hg Sick sinus syndrome without a pacemaker Sinoatrial node block 2nd or 3rd degree AV block without a pacemaker Resting heart rate <60 bpm Atrial pacemaker dependence |
Sinus node disease Cardiac conduction defects Prolonged QT interval |
Dose Adjustments of Sacubitril/Valsartan for Specific Patient Populations
Population |
Initial Dose |
|
High-dose ACEI
|
49/51 mg twice daily |
|
High-dose ARB
|
49/51 mg twice daily |
|
De novo initiation of ARNI OR Low or medium dose ACEI
|
24/26 mg twice daily |
|
Low or medium dose ARB
|
24/26 mg twice daily |
|
ACEI/ARB naive Severe renal impairment (eGFR < 30 mL/min/1,73m2) Moderate hepatic impairment (Child-Pugh Class B) Elderly (age at least 75 years) |
24/26 mg twice daily |
Contraindications and Cautions for Sacubitril/Valsartan
Contraindications |
Cautions |
|
Within 36 hours of ACEI use History of angiodema with or without an ACEI or ARB Pregnancy Lactation (no data) Severe hepatic impairment (Child-Pugh C) Concomitant aliskiren use in patients with diabetes Known hypersensitvity to either ARB or ARNI |
Renal impairment
Hepatic impairment:
Renal arterial stenosis Systolic blood pressure <100 mmHg Volume depletion |
Recommended Indications/Contraindications for Vasodilators [3,4]
Indications |
Contraindications |
Cautions |
|
In self-described African American patients with persistently symptomatic NYHA Class III-IV HFrEF despite optimal GDMT, hydralazine-isosorbide dinitrate combinations can reduce morbidity and mortality |
Hypersensitivity to either agent Concomitant use of phosphodiesterase-5 inhibitors or riociquat (i.e. pulmonary HTN med) |
Volume depletion Hypotension |
Recommended Indications/Contraindications for Cardiac Glycoside [4]
Indications for use of Digoxin |
Contraindications |
Cautions |
|
Can be useful in HFrEF for persistent NYHA Class III and IV symptoms despite optimal guideline directed therapy to reduce hospitalizations for HF [3] May be useful adjunctive therapy to control heart rate in atrial fibrillation In HF, the target steady-state, serum concentration is 0.5 ng/ml to 0.8 ng/ml, preferably obtained prior to receipt of next dose Has narrow toxic to therapeutic window |
Significant sinus or AV block Acute or subacute kidney injury |
Dose adjustments warranted based on ideal body weight and renal function Presence of hypokalemia, hypomagnesemia, or hypercalcemia Use cautiously with other medications that effect sinus or AV nodal function or impact serum digoxin concentration Cardiac amyloidosis |
New Therapies for HFrEF: SGLT-2i (Sodium Glucose Cotransporter-2 Inhibitors
SGLT-2 Inhibitors, which were originally used for diabetic control, now have an increasing role in HFrEF care.
Mechanism: The primary mechanism for glucose regulation of these medications is through inhibition of reabasorption of glucose in the kidney.
Impact: Of note, all 3 SGLT-2i show benefit in HF with DM[8,9]. Please note table below.
Effect of SGLT-2i on Select CV Outcomes in Placebo Controlled Trials [8]
SGLT-2i |
3 Point MACE* Decreased Risk |
HF Hospitalizations Decrease |
|
Canagliflozin (trade: Invokana) |
-14% |
-33% |
|
Dapagliflozin (trade: Farxiga) |
-14% |
-27% |
|
Empagliflozin (trade: Jardiance) |
-17% |
-35% |
*3 Point MACE (events/100 pt-yrs): Major nonfatal stroke, nonfatal MI, CV death, HF hospitalizations. Mean follow-up periods ranged from 18 -50 months across studies. [8]
When to Consider and How to Prescribe
In patients with and without diabetes, with HFrEF or worsening CKD, (Step 4 if still symptomatic on ARNI, B-Blocker, Mineralocorticoid Receptor Antagonist) consider adding a SGLT2 Inhibitor if GFR >30.
If the patient’s HbA1C is < 8% and are taking agents which can cause hypoglycemia (e.g. insulin, sulfonylureas/metaglitinides), their regimen may need to be modified to avoid hypoglycemia. For those with HbA1C > 10%, attention should be paid towards excessive glucosuria induced diuresis and an increased incidence of GU/mycotic infections.
If not able to tolerate or GFR <30, add a Glucagon-like peptide 1 receptor agonists (GLP-1 RAs), which are more easily tolerated without the risk of DKA or amputations.
Of note, a SGLT-2i diabetic medication, Dapagliflozin (Trade: Farxiga), was FDA approved10 in May 2020 for adults with NYHA Class II-IV HFrEF with and without DM to reduce the risk of cardiovascular death and heart failure hospitalizations. In 2019, in the Dapagliflozin And Prevention of Adverse-Outcomes in Heart Failure (DAPA-HF) trial[11], a randomized, double-blind, placebo-controlled study of nearly 5,000 HFrEF patients who received 10 mg daily of dapagliflozin in addition to standard care exhibited fewer cardiovascular deaths, hospitalizations for heart failure, and urgent heart failure visits compared to controls receiving the placebo after 18 months.
26% relative risk reduction and 5% absolute risk reduction for composite outcome of CV death or the worsening of HF (triggering hospitalization or urgent visit requiring IV diuretics).
NNT was 21 for death or hospitalization for HF or urgent visit.
Findings were similar in those with and without diabetes.
Dapagliflozin is covered through a majority of payers. Of note, costs $589 per month ($7,068 annually), without discount12.
Contraindications and Cautions for Dapagliflozin [9,13]
Contraindications |
Cautions |
|
Osteopenia |
HFpEF Considerations
- Consider use of SGLT-2i (GFR >30) or GLP-1 Agonists if SGLT-2i contraindicated
- However, trials ongoing to evaluate impact of SGLT-2i in HFpEF
Vaccinations for Heart Failure Patients
Influenza vaccine |
Recommended for all patients with HF |
Pneumococcal vaccine |
The PPSV23 is recommended for all adult patients with heart failure. Administration of PCV13 should also be considered for patients 65 years old and older. |
Care Delivery Steps & Clinical Integration Models
« Medications Contents Testing & Referrals »
A wide-variety of team members can be involved in the diagnosis, severity classification and care of heart failure. Please see the table below for care delivery steps.
Below are potential team members and options to integrate primary and advanced care for heart failure patients.
Care Delivery Step |
Possible Team Member(s) |
|
Diagnosis and Severity Classification |
Specialist, PCP, APN |
|
Initial Treatment (Medications, Nutrition, Vaccines) |
Specialist, PCP, APN, Pharmacy |
|
Maintenance Treatment (Medication Adjust/Adherence, Nutrition, Vaccines) |
Specialist, PCP, APN, Pharmacy |
|
Self-Management (Weight monitoring/ Symptom response, Motivational Interviewing) |
Pharmacy, Care Management (RN), Health Coaches, Certified Diabetes Educators |
|
Coordinate Specialty Treatment or Testing/Advanced Care |
Care Management (SW, RN) |
|
Behavioral Health (Screen and Refer/Initiate Treatment) |
PCP, APN, Pharmacy, LCSW (If available) |
|
Care Management/Home Care Services |
CM (RN, SW), Home Health Aide, Community Paramedicine |
|
Telemonitoring/Home Care Services |
Specialist, Care Management (RN), Home Health Aide |
|
Palliative Care (screening) |
Specialist (Cardiologist, Pulmonologist, or Palliative Care), PCP, APN, Pharmacy, Care Management (RN) |
Team Member Acronym Legend
PCP |
Primary Care Provider |
APN |
Advanced Practice Nurse |
RN |
Registered Nurse |
LCSW |
Licensed Clinical Social Worker |
SW |
Social Worker |
Testing & Referral
« Care Delivery Steps & Clinical Integration Models Contents Initial and Subsequent Office Visit Templates »
Use of BNP in Heart Failure [3]
B-type natriuretic peptide (BNP) and N-terminal pro–B type natriuretic peptide (NT-proBNP) are the most studied biomarkers in heart failure.
BNP is released in direct relationship to myocardial wall stress and plays a role in diagnosis and prognostication.
Higher concentrations of BNP or NT-proBNP in an ambulatory patient with HFrEF informs high risk, particularly when the concentrations are rising. Current clinical practice guidelines give a Class I recommendation to measure NT-proBNP or BNP to support a clinical diagnosis of HF, to assess disease severity, or to establish prognosis.
More recently, biomarkers have been examined for their role as a marker of clinical responsiveness to GDMT for HFrEF. Patients whose natriuretic peptide concentrations do not fall with GDMT (“nonresponders”) have a worse prognosis.
Measurement can support clinical judgment with respect to prescription of GDMT, and to provide helpful objective data regarding decision-making for referral to advanced HF therapies. In the setting of worsening symptoms, the reassessment of BNP or NT-proBNP may be informative.However, serial assessment of BNP or NT-proBNP to guide aggressive titration of GDMT is not indicated and not warranted.
Several factors may interfere with the interpretation of natriuretic peptide concentrations:
- Severe renal dysfunction
- Sacubitril/valsartan (Entresto) will increase BNP levels due to neprilysin inhibition, and concentrations tend not to return to baseline despite chronic therapy. BNP concentrations will increase (while NT-proBNP will most often fall) with ARNI therapy, and thus it may be more prudent to check only NT-proBNP in patients on ARNI.
- Also, transient increases in natriuretic peptide levels have been documented in the initial phases of beta-blocker initiation; such changes should not preclude up-titration of beta-blocker therapy, which should be guided by patient tolerance instead of asymptomatic change in natriuretic peptide levels.
HFpEF BNP Consideration
Absolute values are lower than in HFpEF, with up to 30% of HFpEF patients having normal levels[15]
HFpEF Evaluation and Testing Considerations[15,16]
Consider Amyloidosis (Red Flag Sxs- Carpal Tunnel, Spinal Stenosis, Neuropathy). Note: High baseline BNP levels and serum troponin concentrations are highly suggestive of cardiac amyloidosis, allowing differentiation from other etiologies of cardiac hypertrophy. In cardiac amyloid, the electrocardiogram may show low voltages despite the presence of ventricular hypertrophy on the echocardiogram.
If etiology of HFpEF remains unclear consider Rheumatologic causes (Scleroderma, Sarcoidosis, Connective Tissue Disease).
Cardiac imaging plays an important role in diagnosis:
- Echocardiogram: EF>50%, LVH, pulmonary hypertension, and evidence of significant diastolic dysfunction are common findings
- Cardiac MRI: useful in evaluating myocardial extracellular volume, detecting infiltrative processes, and assessing scar burden (2013 guideline)
- Technetium pyrophosphate scanning can be useful in the evaluation of patients with suspected cardiac amyloidosis
Cardiac catheterization: invasive hemodynamic assessment of LV, RV, and pulmonary artery pressures, at rest and with exercise, and endomyocardial biopsy are helpful when noninvasive evaluation is inconclusive.
RHF Evaluation and Testing Considerations[5]
RHF impairs LV filling leading to decreased Stroke Volume and Cardiac Output, neurohormonal activation, salt and water retention, increased central venous pressure, systemic venous hypertension, congestive hepatopathy and cardiorenal syndrome.
- Cardiorenal Syndrome: Increased CVP and renal vein pressure and decreased cardiac output lead to renal dysfunction
- Cardiohepatic Syndrome: Due to hepatic congestion and decreased perfusion. May lead to cirrhosis.
When to Refer to a Specialist
-
New-onset HF (regardless of EF): Refer for evaluation of etiology, guideline-directed evaluation and management of recommended therapies, and assistance in disease management, including consideration of advanced imaging, endomyocardial biopsy, or genetic testing for primary evaluation of new-onset HF
-
Chronic HF with high-risk features, such as development of 1 more of the following risk factors:
-
Need for chronic IV inotropes
-
Persistent NYHA functional class III-IV symptoms
-
Systolic blood pressure at or below 90 mm Hg or symptomatic hypotension
-
Creatinine at or above 1.8 mg/dl or BUN at or above 43 mg/dl
-
Onset of atrial fibrillation, ventricular arrthymias, or repetitive ICD shocks
-
Two or more ED visits or hospitalizations for worsening HF in prior 12 months
-
Inability to tolerate optimally dosed beta-blockers and/or ACI/ARB/ARNU and/or aldosterone antagonists
-
Clinical deterioration, as indicated by worsening edema, rising biomarkers (BNP, NT-proBNP, others), worsened exercise testing, decompensated hemodynamics, or evidence of progressive re-modeling on imaging
-
High mortality risk using a validated risk model for further assessment and consideration of advanced therapies, such as Seattle Heart Failure Model
-
-
To assist with management of GDMT, including replacement of ACEI or ARB therapy with ARNI for eligible patients or to address comorbid conditions such as chronic renal disease or hyperkalemia, which may complicate treatment
-
Persistent reduced LVEF at or below 35% despite GDMT for at least 3 months for consideration of device therapy in those patients without prior placement of ICD or CRT, unless device therapy contraindicated or inconsistent with overall goals of care
-
Second opinion needed regarding etiology of HF; for example:
-
Coronary ischemia and the possible value of revascularization
-
Suspected myocarditis
-
Established or suspected specific cardiomyopathies, e.g., hypertrophic cardiomyopathy, arrhythmogenic right ventricular dysplasis, Chagas disease, restrictive cardiomyopathy, cardiac sarcoidosis, amyloidosis, aortic stenosis.
-
Valvular heart disease and the possible value of valve repair
-
-
Annual review of patients with established advanced HF in which patients/caregivers and clinicians discuss current and potential therapies for both anticipated and unanticipated events, possible HF disease trajectory and prognosis, patient preferences, and advanced care planning
-
Assessment of patient for possible participation in a clinical trial
When to Refer for Device Therapy
Consider EP referral for primary ICD or CRT in patients with EF at or below 35% for at least 90 days (or 40 days post MI) on chronic GDMT
When to Refer to Cardiac Rehab
People of all ages with heart conditions, including HF, can benefit from a cardiac rehab program.
Medicare and most other insurers provide reimbursement for cardiac rehab for HFrEF. Exceptions include cardiac rehab in the wake of procedures to implant a pacemaker or implantable cardioverter defibrillator (ICD). o Coverage after heart failure is usually limited to patients with compromised EF. Specifically, patients with left ventricular ejection fraction of 35% or less and New York Heart Association Class II to IV symptoms with at least 6 weeks of heart failure therapy will be covered. Anyone outside this criteria will not be covered.
Mount Sinai Heart's Cardiac Rehabilitation Program
Cardiac Rehabilitation has substantial benefits in driving outcomes for most patients with Heart Failure. Providers who refer patients can expect a 6-12 weeks (2-3x a week) comprehensive, individualized program, well beyond exercise and diet to include education, counseling, and emotional support, among other services. Program is covered by Medicare, NY State Medicaid, and most commercial plans.
Consider referring patients to Mount Sinai Heart’s Cardiac Rehabilitation Program if patient has the following diagnoses or conditions:
- Stable, HFrEF, with left ventricular ejection fraction of 35% or less and New York Heart Association class II to IV symptoms with at least 6 weeks of heart failure therapy
- Stable angina
- Hx of PCI
- Hx of MI within the preceding 12 months
- Bypass or valve surgery
- Heart Transplant
- Any patients with diabetes who you believe will benefit. (Diabetes alone is not a covered condition/diagnosis but we can encourage them to enroll into our Medical Fitness program).
- Minimal insurance coverage for HFpEF if no other cardiac history.
Refer Patients to:
Mount Sinai Doctors — East 85th Street
234 E 85th Street, Lower Level, New York, NY 10028
212-241-8597
Mount Sinai South Naussau Cardiac Rehabilitation Program
The MSSN Cardiac Rehabilitation Program is a 36 session program where patients commit to coming to the Center every M-W-F for 12 weeks. The program is covered by Medicare and the program accepts NY Medicaid, and most commercial plans. When a referral is made to the Cardiac Rehabilitation Program insurance is verified, authorizations obtained and patients are called to inform them of any copays and out of pocket expenses they will incur.
MSSN Cardiac Rehabilitation program follows CMS strict admissions guidelines for Outpatient Cardiac Rehabilitation. Listed below are the diagnoses that are accepted:
- An acute myocardial infarction within the preceding 12 months
- A coronary artery bypass surgery
- Current stable angina pectoris
- Heart valve repair or replacement
- Percutaneous transluminal coronary angioplasty or coronary stenting
- A heart or heart-lung transplant
- Heart Failure Note: Stable, chronic heart failure is defined as patients with left ventricular ejection fraction of 35% or less and New York Heart Association (NYHA) class II to IV symptoms despite being on optimal heart failure therapy for at least 6 weeks
Refer Patients to:
Mount Sinai South Nassau
440 Merrick Road, Oceanside NY 11572
516-255-8280
Suggested Actions for Managing Comorbities in Heart Failure Patients
Managing Comorbidities of Heart Failure
Comorbidity |
Association with Heart Failure Outcomes |
Clinical Trial Evidence for Modulating Comorbidity |
Suggested Action |
|
Cardiovascular |
|
|
|
|
Coronary Artery Disease |
Strong |
Strong |
Evaluate and revascularize in appropriate patients |
|
Atrial Fibrillation/Flutter |
Strong |
Intermediate |
Treat according to current ACC/AHA/HRS Guideline for the Management of Patients with A-Fib |
|
Mitral Regurgitation |
Strong |
Intermediate |
Refer to structural heart disease expert & treat according to current AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease. Consider transcatheter intervention in carefully selected patients with symptomatice HF and secondary MR. |
|
Aortic Stenosis |
Strong |
Strong |
Refer to structural heart disease expert & treat according to current AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease |
|
Hypertension |
Uncertain |
Strong for Prevention |
Treat according to ACC/AHA hypertension guidelines |
|
Dyslipidemia |
Uncertain |
Strong for Prevention |
Treat according to ACC/AHA Guidelines on the Treatment of Blood Cholesterol and the ACC ECDP on the Role of Non-Statin Therapies for LDL-Cholesterol Lowering in the Management of ASCVD Risk |
|
Peripheral Vascular Disease |
Uncertain |
None |
Treat according to current AHA/ACC vascular guidelines |
|
Cerebrovascular Disease |
Moderate |
Weak |
Treat according to current AHA stroke guidelines |
|
Noncardiovascular |
|
|
|
|
Obesity |
Moderate (inverse association) |
Weak |
Further data needed |
|
Chronic Lung Disease |
Strong |
Weak |
Optimize therapy, consider pulmonary consultation, smoking cessation |
|
Diabetes Mellitus |
Strong |
Intermediate |
Optimize therapy, consider SGLT-2i, consider endocrine consult & follow current American Diabetes Association Standards of Medical Care in Diabetes |
|
Chronic Renal Disease |
Strong |
Weak |
Optimize RAASi therapy, consider nephrology consult, administer SGLT2 inhibitor, use hydralazine/ISDN if ARNI/ACEI/ARB cannot by used |
|
Anemia |
Moderate |
Weak |
Evaluate secondary causes, consider transfusing in severe cases |
|
Iron Deficiency |
Strong |
Intermediate |
Consider intravenous iron replacement for symptom improvement in NYHA Class II and III and iron deficiency (ferritin <100 mg/mL or 100 to 300 ng/mL if transferrin saturation is <20%), to improve functional status and QoL |
|
Thyroid Disorder (hypo or hyper) |
Strong |
Weak |
Consider referral to endocrinologist and/or treatment |
|
Sleep Disordered Breathing |
Strong |
Intermediate |
Consider sleep study and treat severe obstructive sleep apnea to improve sleep quality, consider referring to sleep specialist. Adaptive servoventilation should not be used in HF patients with central sleep apnea. |
|
Hyperkalemia |
Uncertain, may limit initiation and titration of GDMT |
Weak |
Recommend dietary modifcations, consider treatment with patiromer |
HFpEF Consideration
Management of co-morbid conditions is primary focus of care for HFpEF. Major disease focus areas: Atrial fibrillation, Coronary Artery Disease, Diabetes, Pulmonary Hypertension, Obesity, Cardiac Valvular Disease, Chronic Anemia and Rheumatologic Disease.
Palliative Care [26]
Palliative care is beneficial at any stage of a serious illness27. Palliative care, and the medical sub-specialty of palliative medicine, is specialized medical care for people living with serious illness. It focuses on providing relief from the symptoms and stress of a serious illness. The goal is to improve quality of life for both the patient and their family.
Referral Criteria
Consider a specialty-level palliative care referral for patients who meet any of these criteria:
- NYHA class III/IV symptoms with frequent heart failure readmissions
- Anxiety or depression adversely affecting patient's quality of life or their ability to manage their illness
- Assistance with decision-making regarding advanced therapies (VAD, transplant, home inotropic therapy)
Referral Options for Palliative Care within MSHS
Patients with Congestive Heart Failure may be referred to one of two practices. The services provided at each location are identical; please choose the location that is most convenient to your patient.
To make a referral to the Martha Stewart Center for Living at 1440 Madison Avenue, please call: 212-241-1446
To make a referral to the Martha Stewart Center for Living Downtown at Union Square, please call: 212-844-1712
Remote patient monitoring facilitates care. Strongly consider use of pulmonary artery pressure monitoring (CardioMEMS) to reduce heart failure hospitalization rates.
Remote Patient Monitoring
Remote patient monitoring is important in chronic disease management for select patients.
Connected Hearts Program
-
Using Omron® devices for home blood pressure measurement and weight measurement via Bluetooth data hub transmission to Epic EMR flowsheet
-
Clinical Pharmacist monitoring data and intervening directly with patients on medications, diet and care coordination
CardioMEMS
-
Consider use of pulmonary artery pressure monitoring (CardioMEMS) to reduce heart failure hospitalization rates, for both HFrEF and HFpEF[19]
-
Many current Mount Sinai patients (especially HFpEF and RHF) benefit from this monitoring
Team-Based Care
Pharmacy
Pharmacists are a key part of the care team for chronic disease management including heart failure, diabetes, and COPD. The team of pharmacists is rapidly expanding in primary and specialty care. They are credentialed providers that can prescribe and adjust medications through the Collaborative Drug Treatment Model[20]
Referrals to pharmacists are appropriate for:
- Uncontrolled chronic diseases, such as hypertension, diabetes, heart failure, asthma, COPD
- Polypharmacy
- Medication Reconciliation
- Medication Adherence
Home Health
Referrals for Home Health should be handled through the designated Home Health nurse coordinator, a member of the care management team.The Home Health nurse coordinator will assess the patient’s needs and determine appropriateness of Home Health.Telephonic education and reinforcement can be also be delivered by the Nurse Clinical Coordinator. The Home Health RN will not provide patient interventions, they will refer to the nurse care coordinator, if needed.
Providing Home Health nursing and therapy can promote recovery in vulnerable HF patients with post-hospital syndrome and potentially reduce readmissions[21]. Nursing interventions can include various educational components, including recognition of HF symptoms with an action plan, dietary guidelines, medication management, and weight monitoring.
Care Coordination in Heart Failure at MSHS[22]
The medical complexity inherent in most patients with HF generally requires the involvement of multiple clinicians across many care settings. Interdisciplinary, team-based care may be the most effective approach to complex HF care. Mount Sinai Health Partners Care Management social workers and nurses partner with patients, family caregivers, and providers to identify and address known risk factors that can impact patients’ health. Care Management intervention includes:
- A comprehensive assessment of the patient’s understanding of and ability to manage their illness and the psychosocial issues that impact their care
- Development of a comprehensive care plan to set goals to optimize health and quality of life
Referral criteria may include those with:
- Multiple no-shows
- Unexplained non-adherence to medications, testing or treatment
- Demonstrated difficulty managing symptoms and/or disease processes (including those newly diagnosed)
- Frequent admissions or ED visits that may be preventable with additional support
- Complex family dynamics that deplete the provider
- Difficulty accessing needed community-based care
- A high “worry score” (patients you as the provider are most worried about from visit to visit)
How to Refer to Care Management
Use the MSHP Care Management Referral in Epic (order #391414)
or
Send an email
or
Call 212-241-7228
Providers who refer patients can expect prompt and efficient processing of their referral, communication about referral processing and assignment through the Epic Inbasket, and follow up from clinical staff within one week of assignment.
Behavioral Health [23]
Patients should be screened for depression using the PHQ-2/PHQ-9 and referred to psychiatric services, as indicated, through their current care pathway depending on their clinic.
Individuals with CHF are 2-5 times more likely to have anxiety and depressive disorders compared with the general population[24]. Patients with chronic medical illness and a co-morbid psychiatric diagnosis have poorer quality of life, increased functional disability, and increased mortality, to name a few. Increased recognition of treatment of these comorbid conditions is essential.
Certified Diabetes Educators (i.e. Wellness Coaches)
Certified Diabetes Educators (CDEs) practice at the top of their license. They can help manage patients with both a diagnosis of diabetes and heart failure. CDEs are embedded in primary and specialty care.
Patients receive customized education and strategies to achieve optimal quality of life. CDE engagement includes:
- Assessing and educating patients and caregivers on their health condition(s)
- Cohesive collaboration with the medical team to integrate evidenced-based care into patient’s plan of care
- Ongoing monitoring, real-time support and follow up by the medical team
- Seamless communication amongst the medical team
- Specialty care consultations for high risk patients
- Oversight and training by a Heart Failure Medical Director
- Outcomes evaluation
Community Paramedicine (CP)
Community Paramedicine offers rapid evaluation and in-home treatment for patients with acute symptoms with the goal of stabilizing the patient at home and preventing ED visits. The response is provided by a paramedic with ED physician oversight and telemedicine support. There is a <60 min response time to anywhere in New York City, 24/7. We also offer service to Nassau County, Long Island. Relevant diagnostic tools and medications that can be performed/administered in the home setting include:
-
EKG
-
Vital signs
-
Complete Physical Assessments
-
IV Fluids
-
IV Medications including Lasix, Zofran and more!
-
Pain management
Learn more about this service:
Email Ari Breslauer, MPH, CCEMT-P, Program Director, Community Paramedicine at Ari.Breslauer@mountsinai.org
Who can initiate this service at my practice?
-
Any clinician (including mid-levels and RN’s) can trigger this service for their patient who needs urgent evaluation and treatment at home, with the goal of stabilizing the patient and preventing an ED visit.
Rapid Follow Up Clinics (RFU Clinics)
- RFUs can provide additional post-discharge support
- Treatment in specialized HF clinics using nurse intervention reduces readmission frequencies and improves quality of care for HF patients[25]
- For referrals contact the individuals listed below
MSHS Heart Failure Rapid Follow Up Clinics Referral Contacts
|
Campus |
Primary Contact |
Hours |
Location |
Uses ReDS Vests |
|
The Mount Sinai Hospital |
(212) 241-7300 |
Wednesdays 8:00 am to 5:00 pm, flexible hours upon request |
1190 Fifth Avenue, GP1C |
Yes |
|
Mount Sinai Beth Israel |
Jayitha Janardhanan, NP |
Tuesday 9:00 am to 12:00 pm |
10 Union Square East |
No (coming 2020) |
|
Mount Sinai Queens |
Monday 1:00 pm to 5:00 pm, Tuesday 1:00pm to 5:00pm, Thursday 1:00pm to 2:00 pm, Friday 9:00 am to 12:00 pm |
MSQ Ambulatory Pavilion 2510 30th St., 5th Floor |
Yes, currently for outpatient only |
|
|
Mount Sinai West |
(212) 532-2700 |
Monday thru Thursday 8:00 am to 4:30 pm, Friday 8:00 am to 1:00 pm |
440 West 114th Street, 2nd Floor, Cardiovascular Institute |
Yes |
|
Mount Sinai South Nassau |
Monday thru Friday 11:00 am to 4:00 pm |
One Healthy Way, Oceanside, NY 11572 |
No |
ReDS Vests [25]
MSHS has several vests in use including at Rapid Follow Up clinics. The ReDS vest measures lung fluid in heart failure patients. The vest uses radar technology to measure the % of water in the Right Middle Lobe. It is non-invasive and readings are available within 90 seconds.
Initial and Subsequent Office Visit Templates
« Testing & Referrals Contents References »
Initial Visit: Confirm Diagnosis and Etiology and Initiate Therapy
Provider History
- Duration of illness
- NYHA Class (I-IV)
- Weight gain/loss, new or worsening edema, orthopnea, and dyspnea
- Assessment of comorbidities including obesity, prior CAD, atrial fibrillation, DM, HLD, and smoking
- Potential clues suggesting etiology of heart failure if unknown (ischemic vs. non-ischemic)
- Assess, if indicated, for any known or suspected anemia, valvular, lung, liver, thyroid, renal, or rheumatologic diseases, pulmonary hypertension, sleep apnea, HIV infection, recent pregnancies, relevant travel, or symptoms of pheochromocytoma
- Complete medication review, including OTC medications
- PHQ 2 and if positive, PHQ 9
- Current/past alcohol use
- Prior drug abuse, including IVDA
- Diet and fluid intake
- Family history
- Inquire if Healthcare Proxy form has been completed
- Previous COVID-19 infection and antibody status
Provider Physical
- Blood pressure, pulse, weight, BMO, possibly 02 sat
- Assessment of volume status
- Cardiovascular exam (especially JVD, hepatojugular reflex, and presence of S3)
- Telemedicine consideration: “edema check”: Instruct patient to place fingers where there is swelling on the lower leg, push down hard, and then remove. Ask patient if there is an indentation, and if so, how deep it is.
Diagnostic Studies
Lab work
- CBC with diff
- BMP, magnesium
- Lipid profile
- BNP or NT-proBNP (if no prior documentation)
- Troponin (risk marker)
- Digoxin level, if signs or symptoms of toxicity or recent addition of interacting drug
- PT/INR (Every patient on warfarin should be enrolled in an anticoagulation clinic or have his/her PT/INR followed closely by a designated provider.)
Consider the following in appropriate patients if the etiology of HF is unknown:
- TSH
- LFTs
- HIV Ab (if not recently documented)
- Anemia panel and Hemochromatosis screen (transferrin sat, ferritin)
- Rheumatologic evaluation
- Evaluation for amyloidosis, if red flags present
- Others, as indicated
Procedures
- 12-lead EKG; document QRS duration
- Echo with Doppler flow studies; document EF
- Chest X-ray: PA & Lat
- Ischemic workup in appropriate patients
Telemedicine Considerations
When possible, get blood tests done ~ 1 week prior to virtual visit, either at office, local phlebotomy center (Labcorp/Quest) or have blood drawn at home (Apex Lab). Results of home cardiac rhythm (KardiaMobile) monitoring can be transmitted to practice in advance of visit. Patient should upload results of home monitoring into Epic or fax to office prior to visit. When available, staff can outreach to patient in advance of visit to collect needed information.
Medical Therapy
For patients with HFrEF
Plan to initiate treatment in stepwise manner. Titrate to target dose as per GDMT. If the patient is hemodynamically stable, it is generally acceptable to double the dose of the neurohormonal antagonist (Beta-blockers, ACE, ARB, ARNI mineralocorticoid antagonists (i.e. Spironolactone)) when increasing the dose. It is recommended that only one of these agents be increased each visit. Caution is advised if increasing more than one. Document contraindications or intolerance
ACEI/ARB: initiate/titrate to target dose, document contraindications/intolerance. Use Subcutril/Valsartan (i.e. Entresto) instead of ACE/ARB for patients with NYHA class II-III and LVEF at or below 35% who are stable an an ACEI/ARB.
Beta blocker: initiate/titrate using either carvedilol, sustained-release metoprolol succinate, or bisoprolol
Aldosterone antagonist: initiate/titrate if not contraindicated (GFR>30ml/min,K <5.0 mEq/ml) and NYHA class II-IV HF with LVEF at or below 35% (NYHA Class II should have hx of prior CV hospitalization or elevated BNP) or post-MI with LVEF at or below 40% with symptoms of HF or who have DM
Hydralazine/isosorbide dinitrate: Initiate/titrate in African American patients NYHA class III-IV on standard medical therapy including ACEI/ARB or ARNI, and BB; consider in all patients who cannot tolerate an ACEI/ARB or ARNI unless contraindicated.
Diuretic: initiate/titrate in patients with fluid retention.
Ivabradine: if sinus rhythm, HR >70 bpm on maximally tolerated beta blocker, NYHA II-III, and no contraindications
Digoxin for NYHA III-IV symptoms despite optimal GMT and/or rate control for atrial fib.
Dapagliflozin (ie SGLT-2i) should be considered as adjunctive therapy, to reduce CV death and worsening HF, even in absence of Type 2 diabetes, unless contraindicated, and after considering potential incremental cost to patient
Anticoagulation indicated if atrial fibrillation present. Choice of agent should be individualized. Routine anticoagulation for heart failure without atrial fibrillation is not indicated.
Antiplatelet therapy: as indicated
Lipid-lowering therapy: as indicated
For patients with HFpEF
Focus on treating volume overload (diuretics, salt restriction) and effectively managing their comorbidities. Mineralocorticocoid receptor antagonists may be helpful in HFpEF. Consider use of SGLT-2i (GFR >30) or GLP-1 Agonists if SGLT-2i contraindicated. Avoid nitrates.
Considerations for Patients with Co-existing Type 2 Diabetes
Metformin remains first line therapy for diabetes (if GFR >30). SGLT-2i (dapagliflozin, canaglifozin, empaglifozin) are preferred in HFrEF when additional therapy required, unless contraindicated/cautions {Type 1 DM, symptomatic hypotension or SBP <95 mmHg, GFR <30, prior/high risk for DKA, risk of foot amputation (ulcer, PVD, neuropathy, deformity), recurrent UTI’s/genital mycotic infections}.
Thiazolidinendiones (pioglitazone, rosiglitazone) are contraindicated.
GLP-1 receptor antagonists (exenatide, semaglutide,dulaglutide, liraglutide) can be used if SGLT-2 inhibitors are contraindicated. Contraindications to GLP-1 RA include personal/fam hx of medullary thyroid cancer, MEN Type 2, pancreatitis, gastroparesis, GFR <30. (perhaps remove)
DPP-4 inhibitors (linagliptin, sitagliptin, alogliptin) should be used cautiously in all patients who have diagnosis. Saxagliptin should not be used.
Immunizations
Pneumococcal vaccination (PPSV-23 and possibly PV-13) and annual influenza vaccination in the absence of known contraindications. For telemedicine visits, can be ordered and subsequently administered in office or at local pharmacy.
Device Therapy
Remote monitoring of BP, pulse, weight, possibly 02 sat.
Consider EP referral for primary ICD or CRT in patients with EF less than or equal to 35% for at least 90 days (or 40 days post MI) on chronic GDMT.
Escalation Pathway
Primary Care: Every patient should have a primary care physician (Patients should be seen at least quarterly by PCP or Cardiologist.)
Cardiology: All new diagnoses of heart failure, assistance desired with GDMT, including replacement of ACEI/ARB w ARNI, and/or other significant co-existing cardiac disorders
Advanced Heart Failure: Refer patients if refractory symptoms or end stage heart failure, (acronym “I-NEED-HELP”)
Cardiac Rehabilitation: If stable HFrEF, EF <35%, NYHA III-IV despite 6 weeks of HF therapy.
Other Referrals to Consider
Sleep Medicine Referral if coexisting obstructive sleep apnea
Care Management referral: frequent ED visits and hospitalizations, multiple no shows, non-adherence to treatment plan, complex psychosocial issues impacting care, difficulty accessing community resources
Pharmacist referral (if available): uncontrolled HF, non-adherence to medications, polypharmacy, poorly controlled comorbid diseases, med reconciliation
Home Health referral: particularly for recently discharged, vulnerable HF patients
Behavioral Health referral: active psychiatric disorders adversely impacting heart failure care, not manageable in primary care setting
Wellness Coaches (CDE): for patients with co-existing diabetes
Remote patient monitoring for select patients: Connected Hearts Program and Cardiomems
Palliative Care referral for NYHA III-IV with frequent admissions, significant anxiety and depression, and assistance with decision-making regarding advanced therapies (LVAD, transplant, home ionotropic therapy)
Device Therapy
Remote monitoring of BP, pulse, weight, possibly 02 sat.
Consider EP referral for primary ICD or CRT in patients with EF less than or equal to 35% for at least 90 days (or 40 days post MI) on chronic GDMT.
Patient Education
Provide patient/family with the heart failure education booklet, “Managing Your Heart Health”, and other general information about heart failure.
Technique to measure and record blood pressure, pulse, weight, 02 sat at home
How to record and transmit cardiac rhythm, for those with afib/flutter. (KardiaMobile)
How to access mychart and any desired clinical apps
Diet/Fluids
Limit salt intake to <3 grams/day
Other diets as indicated
Fluid restriction <2 L/day (6-8 glasses) for patients with moderate hyponatremia (serum sodium <130 mEq/L) and should be considered in other patients to assist in treatment of fluid overload
Subsequent Follow-Up Visits
Provider History
- NYHA Class (I-IV)
- Document etiology of heart failure
- Interval history including recent ED visits, hospitalization, weight changes, new/worsening HF symptoms
- Reassessment of status of medical comorbidities
- Complete medication review and assessment of compliance
- Determine if Healthcare Proxy form has been completed previously
Provider Physical
- Blood pressure, pulse, weight, BMO, possibly 02 sat
- Assessment of volume status
- Cardiovascular exam (especially JVD, hepatojugular reflex, and presence of S3)
- Telemedicine consideration: “edema check”: Instruct patient to place fingers where there is swelling on the lower leg, push down hard, and then remove. Ask patient if there is an indentation, and if so, how deep it is.
Diagnostic Studies
Lab work as necessary
- BMP: check 1-2 weeks after dose titration of ACEI/ARB or spironolactone/eplerenone
- Magnesium: if on diuretic, check at same interval as BMP
- BNP or NT-proBNP if volume stats unclear
- Digoxin level, if signs or symptoms of toxicity or recent addition of interacting drug
- PT/INR (Every patient on warfarin should be enrolled in an anticoagulation clinic or have his/her PT/INR followed closely by a designated provider.)
Procedures
- Repeat echo if significant change in clinical status, recent clinical event, on GDMT that may significantly affect cardiac function, or may be candidates for device therapy
- Consider cardiac MRI if cause of HFpEF or RHF unclear
Telemedicine Considerations
When possible, get blood tests done ~ 1 week prior to virtual visit, either at office, local phlebotomy center (Labcorp/Quest) or have blood drawn at home (Apex Lab). Results of home cardiac rhythm (KardiaMobile) monitoring can be transmitted to practice in advance of visit. Patient should upload results of home monitoring into Epic or fax to office prior to visit. When available, staff can outreach to patient in advance of visit to collect needed information.
Medical Therapy
For patients with HFrEF
Escalate treatment in stepwise manner. Titrate to target dose as per GDMT. If the patient is hemodynamically stable, it is generally acceptable to double the dose of the neurohormonal antagonist (Beta-blockers, ACE, ARB, ARNI mineralocorticoid antagonists (i.e. Spironolactone)) when increasing the dose. It is recommended that only one of these agents be increased each visit. Caution is advised if increasing more than one.By end of Visit #2, each patient should be on both a beta-blocker and either an ACEI or an ARB. Document contraindications or intolerance.
ACEI/ARB: initiate/titrate to target dose, document contraindications/intolerance. Use Subcutril/Valsartan (i.e. Entresto) instead of ACE/ARB for patients with NYHA class II-III and LVEF at or below 35% who are stable an an ACEI/ARB.
Beta blocker: initiate/titrate using either carvedilol, sustained-release metoprolol succinate, or bisoprolol
Aldosterone antagonist: initiate/titrate if not contraindicated (GFR greater than or equal to 30ml/min,K <5.0 mEq/ml) and NYHA class II-IV HF with LVEF at or below 35% (NYHA Class II should have hx of prior CV hospitalization or elevated BNP) or post-MI with LVEF at or below 40% with symptoms of HF or who have DM
Hydralazine/isosorbide dinitrate: Initiate/titrate in African American patients NYHA class III-IV on standard medical therapy including ACEI/ARB or ARNI, and BB; consider in all patients who cannot tolerate an ACEI/ARB or ARNI unless contraindicated.
Diuretic: initiate/titrate in patients with fluid retention.
Ivabradine: if sinus rhythm, HR >70 bpm on maximally tolerated beta blocker, NYHA II-III, and no contraindications
Digoxin for NYHA III-IV symptoms despite optimal GMT and/or rate control for atrial fib.
Dapagliflozin (ie SGLT-2i) should be considered as adjunctive therapy, to reduce CV death and worsening HF, even in absence of Type 2 diabetes, unless contraindicated, and after considering potential incremental cost to patient
Anticoagulation indicated if atrial fibrillation present. Choice of agent should be individualized. Routine anticoagulation for heart failure without atrial fibrillation is not indicated.
Antiplatelet therapy: as indicated
Lipid-lowering therapy: as indicated
For patients with HFpEF
Continue to treat any volume overload (diuretics, salt restriction) and optimize control of comorbidities. Consider mineralocorticocoid receptor antagonists. Consider use of SGLT-2i (GFR >30) or GLP-1 Agonists if SGLT-2i contraindicated. Avoid nitrates.
Considerations for Patients with Co-existing Type 2 Diabetes
Metformin remains first line therapy for diabetes (if GFR >30). SGLT-2i (dapagliflozin, canaglifozin, empaglifozin) are preferred in HFrEF when additional therapy required, unless contraindicated/cautions {Type 1 DM, symptomatic hypotension or SBP <95 mmHg, GFR <30, prior/high risk for DKA, risk of foot amputation (ulcer, PVD, neuropathy, deformity), recurrent UTI’s/genital mycotic infections}.
Thiazolidinendiones (pioglitazone, rosiglitazone) are contraindicated.
GLP-1 receptor antagonists (exenatide, semaglutide,dulaglutide, liraglutide) can be used if SGLT-2 inhibitors are contraindicated. Contraindications to GLP-1 RA include personal/fam hx of medullary thyroid cancer, MEN Type 2, pancreatitis, gastroparesis, GFR <30. (perhaps remove)
DPP-4 inhibitors (linagliptin, sitagliptin, alogliptin) should be used cautiously in all patients who have diagnosis. Saxagliptin should not be used.
Immunizations
Pneumococcal vaccination (PPSV-23 and possibly PV-13) and annual influenza vaccination in the absence of known contraindications. For telemedicine visits, can be ordered and subsequently administered in office or at local pharmacy.
Device Therapy
Remote monitoring of BP, pulse, weight, possibly 02 sat.
Consider EP referral for primary ICD or CRT in patients with EF less than or equal to 35% for at least 90 days (or 40 days post MI) on chronic GDMT.
Escalation Pathway
Primary Care: Every patient should have a primary care physician (Patients should be seen at least quarterly by PCP or Cardiologist.)
Cardiology: All new diagnoses of heart failure, assistance desired with GDMT, including replacement of ACEI/ARB w ARNI, and/or other significant co-existing cardiac disorders
Advanced Heart Failure: Refer patients if refractory symptoms or end stage heart failure, (acronym “I-NEED_HELP”)
Cardiac Rehabilitation: If stable HFrEF, EF <35%, NYHA III-IV despite 6 weeks of HF therapy.
Other Referrals to Consider
Sleep Medicine Referral if coexisting obstructive sleep apnea
Care Management referral: frequent ED visits and hospitalizations, multiple no shows, non-adherence to treatment plan, complex psychosocial issues impacting care, difficulty accessing community resources
Pharmacist referral (if available): uncontrolled HF, non-adherence to medications, polypharmacy, poorly controlled comorbid diseases, med reconciliation
Home Health referral: particularly for recently discharged, vulnerable HF patients
Behavioral Health referral: active psychiatric disorders adversely impacting heart failure care, not manageable in primary care setting
Wellness Coaches (CDE): for patients with co-existing diabetes
Remote patient monitoring for select patients: Connected Hearts Program and Cardiomems
Palliative Care referral for NYHA III-IV with frequent admissions, significant anxiety and depression, and assistance with decision-making regarding advanced therapies (LVAD, transplant, home ionotropic therapy)
Device Therapy
Remote monitoring of BP, pulse, weight, possibly 02 sat.
Consider EP referral for primary ICD or CRT in patients with EF less than or equal to 35% for at least 90 days (or 40 days post MI) on chronic GDMT.
Patient Education
Review recommendations, assess knowledge, treatment adherence; identify/address barriers, needs of patient/ family
Reinforce technique to measure and record blood pressure, pulse, weight at home, 02 sat as indicated
Diet/Fluids
Emphasize importance of daily weights
Assess dietary compliance
Assess adherence to fluid restriction, as indicated
References
This document was written in consultation with Mount Sinai Health System heart failure subject matter experts.
[1] Horwich TB and Fonarow GC. Prevention of Heart Failure. JAMA Cardiol. 2017 Jan 1;2(1):116.
[2] Ponikowski P, Voors AA, Anker SD et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016 Jul 14;37(27):2129-2200.
[3] Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America Circulation. 2017 Aug 8;136(6):e137-e161. Hereafter referred to as the “2017 Heart Failure Pathway.”
[4] Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: Executive Summary. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, circulation 2013;128:1810. Hereafter referred to as the “2013 Heart Failure Pathway.”
[5]Konstam MA, Kiernan MS, Bernstein D et al. Evaluation and Management of Right-Sided Heart Failure A Scientific Statement From the American Heart Association. Circulation. 2018;137:e578–e622
[6] Felker GM, Ellison DH, Mullens W, et al. Diuretic Therapy for Patients With Heart Failure: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75(10):1178-1195.
[7] Diuretics, Loop, In Epocrates for apple IOS software. [Mobile Application Software], retrieved June 18, 2020
[8] Seferovic PM, Coats AJS, Ponikowski P, et al. European Society of Cardiology/Heart Failure Association position paper on the role and safety of new glucose-lowering drugs in patients with heart failure. Eur J Heart Fail. 2020;22:196-213.
[9]Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2018;61:2461–2498.
[10]FDA approves new treatment for a type of heart failure. FDA. 5 May 2020. Updated 22 May 2020. https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-type-heart-failure
[11]McMurray JV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019;381(21):1995-2008.
[12] www.goodRx.com. Accessed 2 June 2020.
[13]Colucci WS. Secondary pharmacologic therapy in heart failure with reduced ejection fraction (HFrEF) in adults. UpToDate. 14 April 2020. Accessed 17 June 2020. https://www.uptodate.com/contents/secondary-pharmacologic-therapy-in-heart-failure-with-reduced-ejection-fraction-hfref-in-adults
[14]Matanock A, Lee G, Gierke R, et al. Use of 13-Valent Pneumococcal Conjugate Vaccine and 23-Valent Pneumococcal Polysaccharide Vaccine Among Adults Aged >=65 Years: Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2019;68:1069–1075.
[15]Henning RJ. Diagnosis and treatment of heart failure with preserved left ventricular ejection fraction World J Cardiol 2020 January 26; 12(1): 7-25
[16] Wolfson AM, Shah KS, Patel JK. Amyloid and the Heart. Current Cardiology Reports (2019) 21: 164.
[17] Department of Cardiology, Mount Sinai Health System
[18] American Heart Association: Am I Eligible for Cardiac Rehab: https://www.heart.org/en/health-topics/cardiac-rehab/am-i-eligible-for-cardiac-rehab
[20] Academy of Managed Care Pharmacy, Practice Advisory on Collaborative Drug Therapy Management, https://www.amcp.org/sites/default/files/2019-03/Practice%20Advisory%20on%20CDTM%202.2012_0.pdf, accessed online July 28, 2020
[21] Jones CD, Bowles KH, Richard A, Boxer RS, Masoudi FA. High-Value Home Health Care for Patients With Heart Failure: An Opportunity to Optimize Transitions From Hospital to Home. Circulation. 2017;10(5):e003676.
[22] Information developed and provided by the Mount Sinai Care Management Department
[23] Information developed and provided by the Mount Sinai Department of Psychiatry
[24] Ratcliff, Chelsea & Fletcher, Terri & Petersen, Nancy & Sansgiry, Shubhada & Kauth, Michael & Kunik, Mark & Stanley, Melinda & Cully, Jeffrey. (2017). Recognition of anxiety, depression, and PTSD in patients with COPD and CHF: Who gets missed?. General Hospital Psychiatry. 2017;47:61-67
[25] Gustafsson F, Arnold JMO, Heart failure clinics and outpatient management: review of the evidence and call for quality assurance, European Heart Journal, 2004;25(18):1596–1604
[26] Information developed and provided by the Mount Sinai Brookdale Department of Geriatrics and Palliative Medicine
[27] Center to Advance Palliative Care; Serious Illness Quality Alignment HUB: State Palliative Care Definitions and Standards. Available at: https://www.capc.org/documents/133/
